Polypharmacy in the United States amongst geriatric healthcare recipients, and its adverse outcomes, have been well researched. The most common negative effects include falls, cognitive impairment, costly emergency room visits, and hospitalizations; age-related changes such as diminished metabolism and drug clearance elevate risk. Additionally, for older adults who receive care in congregate settings such as skilled nursing facilities or assisted living communities, medication volume compounds risk due to medication errors and the possibility of adverse drug situations. Significant numbers of medications create challenges for nursing staff in evaluating medication responses. The coexistence of several chronic conditions in the elderly makes them vulnerable to the risks associated with polypharmacy.
Aspire Clinical Intelligence defines polypharmacy for this population as the use of multiple medications within one of two categories: general polypharmacy and uncontrolled polypharmacy. General polypharmacy is the use of 5 or more drugs, while uncontrolled polypharmacy can be defined as the use of 10 or more drugs. Through extensive research since 2014, Aspire has determined that the average number of prescribed medications for seniors in assisted living is 12 per resident.
Recent health research (beginning in 2021) of a random sample of assisted living residents reveals an average number of medications per individual of 11.2 per day. These same residents had an average of 2.1 falls per resident in 90 days, with a total average of 4.1 falls per resident within 12 months. 46% of this group is cognitively impaired, as evidenced by cognitive evaluation using the St. Louis University Mental Status Examination (SLUMS). The average SLUMS score for the whole group was 17.9. The average SLUMS score for those with 20 or below is 12. Note – The SLUMS examination is for detecting mild cognitive impairment and dementia on a scale of 0 to 30. Scores of 27 to 30 are considered normal in a person with a high school diploma. Scores between 21 and 26 suggest mild neurocognitive disorder. Scores of 0 to 20 indicate dementia.
Aspire Clinical Intelligence is committed to exploring technological opportunities to reduce the number of medications used by this population. Technologies to assist in prescribing, administering, tracking, and monitoring this group are essential. Medications are over-utilized, particularly for those aged 65 and older. Polypharmacy is a systemic problem in how drugs are prescribed and managed. The system needs disruption.
Products and Services Available:
Aspire Clinical Intelligence, LLC is a source code for improving senior population health. Using substantiated clinical facts and standardized protocols, Aspire supports and drives actionable multidisciplinary healthcare decisions. This platform combines historical and real-time health information obtained from direct clinical observation and robust application programming interfaces (API) with existing electronic health records, health-related application software, and biomedical technologies.

The platform is a critical tool for managing the quality and cost of healthcare services, and supports access to the right healthcare services at the right place and at the right time. The effective application of the dynamic health record results in improved outcomes and reduced hospital visits and readmission. A broader application provides valuable information for big data applications and predictive clinical analytics and predictive medicine.
By conducting significant health research into high-impact incidents, including falls, weight loss, infections, ER visits, and hospitalizations, Aspire has concluded that polypharmacy is a leading root cause.
Key Findings #1
Per the CDC, the aging population in the United States will grow exponentially in the coming years. This coupled with the shrinking labor force in the healthcare industry, especially nurses, sets the stage for adverse outcomes associated with polypharmacy. The CDC also suggests elderly individuals taking more than four medications are at increased risk of falls and other negative outcomes.
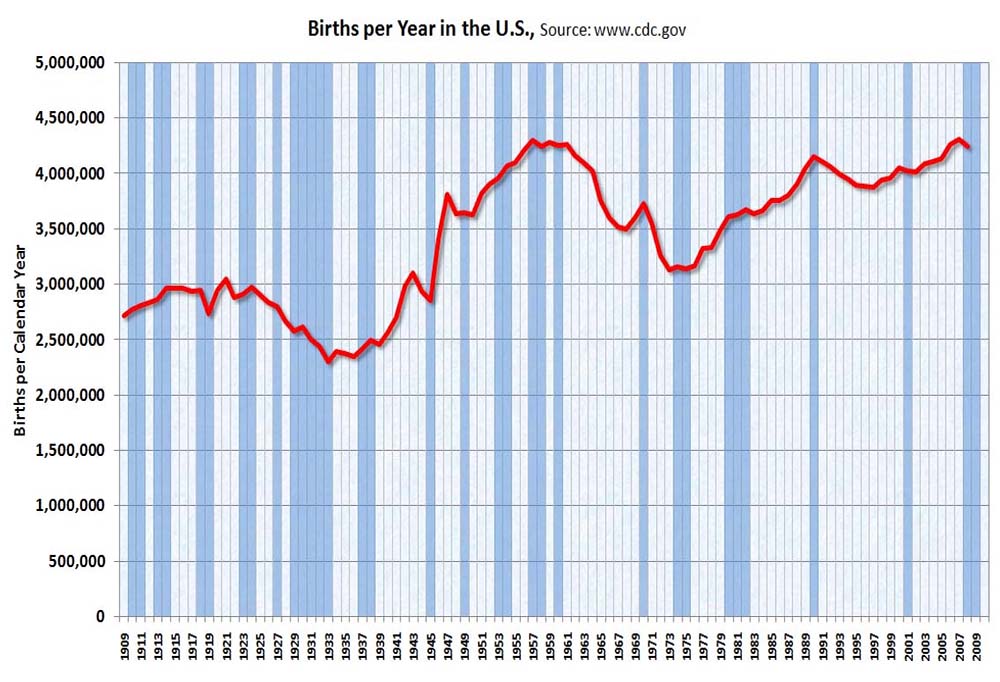
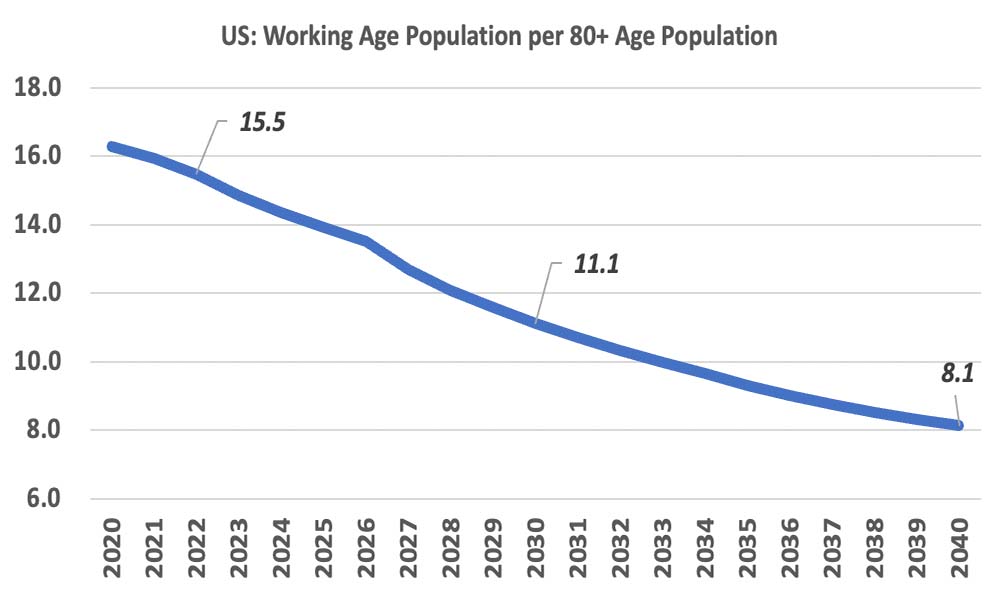
The number of births in the US grew substantially from 1946 to 1964 (baby boomers). This was followed by a steep drop-off in births from 1965 to 1980 (Gen X). These trends have largely resulted in two factors that will greatly impact healthcare and the economy (see graphs below).
A 30% increase in the 65+ population between 2020 and 2030 will result in many more individuals needing healthcare services, and greatly increase the cost of healthcare and medications to society.
A roughly 30% drop in the ratio of the working population to the 80+ population means there will be fewer individuals to care for our seniors, and fewer people in the workforce to pay for medications.
According to data from IntelyCare, a nursing agency, nursing schools graduate 188,000 new nurses each year, but by their second year in the workforce, 33% leave the profession due to burnout (IntelyCare, Nov. 2021).
Key Findings #2
Aspire conducted health research on 237 assisted living residents in early 2022. Records were randomly selected for residents with recent high-impact incidents (falls, infections, and actual or suspected weight loss and malnutrition). Specific to falls, the clinical analysis revealed likely correlations of the root causes below for residents with a history of one or more falls during the first quarter of 2022. Uncontrolled Polypharmacy (10 or more medications) was present in 100% of the cases reviewed.

Orthostatic Hypotension
A review of 49 health records, selected at random for assisted living residents who had experienced one or more falls in January 2022, showed the prevalence of possible orthostatic risk in 47% of the incidents with historical systolic and diastolic blood pressure drops, as evidenced by drops in systolic pressure of 20 mmHg or more and 10 mmHg drops in diastolic blood pressure. Cardiovascular disorders are common causes of falls, and per the CDC, orthostatic hypotension is the most prevalent, affecting up to 68% of institutionalized elderly vs. 6% living independently. Orthostatic hypotension can be caused by adrenal insufficiency, age, and fluid loss, but commonly by medications. Taking antihypertensive medications can increase the risk of orthostatic hypotension.
Cardiac Arrhythmias
26% of this group has a diagnosis of cardiac arrhythmia. The most prevalent arrhythmia is atrial fibrillation (A-Fib) in 66% of cases. A UK study conducted in 2016 evaluated unexplained falls in the elderly and found that 20% of the participants experienced a detectable cardiac arrhythmia attributable to their fall. The study also concluded, “Patients who had a cardiac arrhythmia detected were more likely to experience further falls.”
Depression and the Use of Antidepressants
The average number of falls in 90 days for the cases reviewed is 2.1. When healthcare consumers with a diagnosis of diabetes were isolated, the average number of falls in 90 days triples to 6.4 when the use of one or more antidepressants is noted.
Key Findings #3
Scheduled and PRN Medication Findings
The average number of scheduled medications for this group is 11.2. The average number of available medicines, including scheduled and as-needed (PRN) medications, is 19.3. Each medication regimen contains an average of 4.3 fall risk-increasing drugs (FRIDs). Of the 7.9 available PRN medications, usage was only 1.3 in 90 days, representing an opportunity to significantly save money for Medicare, private insurance, and out-of-pocket costs by consumers.
These correlations, including polypharmacy, represent a significant opportunity for technology applications and further research and development of sophisticated biometric monitoring.
Other opportunities include:
- Enhanced automation in medication delivery and administration
- Improved biometric devices
- Improved health analytics
- Applications of predictive clinical analytics

Medication Waste
Medication waste in congregate living settings is prolific. Medications are pulled from general distribution for several reasons, but most often for discontinuation, discharge, or death. These medications are typically placed into locked, central storage and disposed of per the policy of the institution. A 4,000-bed senior living community wastes an average of 1,000,000 medications annually. Aspire found an average of 50% of PRN medications are not used but are paid for regularly. The financial cost of medication waste is $1,200,000 annually for a 4,000-bed portfolio, and includes roughly $166,000 in out-of-pocket costs paid for by seniors or their families. With more than 1,000,000 people living in assisted living facilities, the cost of medication wastage in the senior living industry is $300,000,000 per year.

In conclusion:
Per the CDC, older adults filled 7.8 billion prescriptions in a span of 18 years for medications that increased fall risk; most of these contribute to orthostatic hypotension and cognitive changes, induce general decline, and contribute to falls. 94% of seniors in the US take medications that increase their risk of falling; 36 million per year, according to the CDC. This is an increase from 57% two decades ago. Within 12 months of a major bone fracture, one-third of adults die. This statistic is associated primarily with hip fractures. Polypharmacy is a significant issue in the United States and is strongly tied to fall rates, costs, and adverse events. Medical costs of falls are estimated at $50 billion annually.
Polypharmacy contributes to falling rates in the elderly, which results in financial impacts on the American healthcare system. Significant contributions are made by private insurance and federal programs, and out-of-pocket by consumers.
If you’d like to learn more about the services and products available from Aspire Clinical Intelligence, please reach out to us at info@aspire1ci.com.
Sources
CDC Fall Death Rates in the U.S. www.cec.gov/HomeandRecreationalSafety
The U.S. Pharmacist 3/31/2021 Are Fall-Risk-Increasing Drugs Behind an Increase in Fall Deaths in Older Adults? https://www.uspharmacist.com/article/are-fallrisk-increasing-drugs-behind-an-increase-in-fall-deaths-in-older-adults
